Public-private partnership: New model for healthcare
As we look forward to a healthcare system that can provide citizens throughout the country affordable, high-quality healthcare, the lessons from the Charikot experience must be heeded
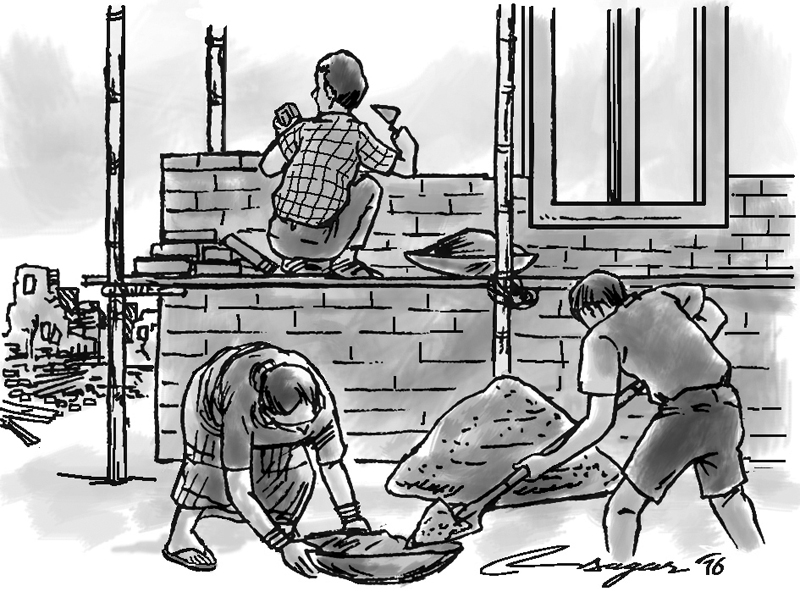
Following the massive earthquake on 12 May, 2015, the healthcare system of Dolakha district was devastated. Forty-six of fifty-four health posts were damaged, and further damage was sustained by both Jiri Hospital and Charikot Primary Health Center.
The Ministry of Health (MoH) offered short-term contracts to NGOs to assist with the reconstruction of health posts – Nyaya Health Nepal (NHN), known for their public-private partnership (PPP) running Bayalpata Hospital in Achham district, committed to this endeavor.
Further negotiations led to a PPP for NHN to manage and expand services at Charikot Primary Health Center. This PPP was historic for the country as it was the first time an NGO assumed management of service delivery at a functioning government healthcare facility.
The PPP began on 24 January, 2016, and we are proud to now celebrate one year of services together.
Public-private partnerships, as described in the Ministry of Finance’s PPP Policy (2015), provide significant value in the form of enhanced quality of services, reduced costs, increased productivity, improved leverage of limited governmental resources, and risk-sharing distributed across private and public-sector partners.
Nepal has successfully utilized the PPP model in multiple sectors, however there is limited experience with PPP in healthcare. Benefits of the PPP model specifically in healthcare include the creation of a division between the purchaser of healthcare services, and the healthcare provider, which has been shown to improve care quality and enhance cost-effectiveness.
The 2015 Constitution guarantees the right to healthcare for all Nepali citizens, however public sector healthcare systems have been insufficiently resourced to provide for this right. In this context, the PPP model offers great potential.
Globally there are many successful examples of PPPs in healthcare, which have been utilized to expand health service delivery in countries around the world.
The first year of PPP management at Charikot has been successful, with greatly expanded healthcare services and improved quality, though there have also been significant challenges. We now reflect on the lessons we have learned as we look forward to the opportunity PPP offers our healthcare system, and citizens across Nepal in need of better healthcare.
Prior to PPP, implementation services at Charikot included OPD, lab, x-ray, and delivery services. The INGO Médecins Sans Frontières (Doctors Without Borders) was instrumental in initial service implementation following the earthquakes, in close partnership with DHO; delivery services were supported by UNICEF during the same period.
Following the immediate post-earthquake period, under PPP management, services available and service utilization have expanded significantly.
Among other expansions, this has included an over five-fold increase in OPD services, three-fold increase in delivery services, fully functioning surgical services and an inpatient department, as well as the first public-sector electronic health record (EHR), and other innovative public health programs.
All services provided under PPP management are free to patients – the PPP is non-profit. Other important successes include:improved quality of healthcare services – including expanded staffing, with more advanced training and skill sets, regular monitoring of quality metrics bolstered by quality improvement initiatives, and services focused upon patient satisfaction and dignity and improved staff management structures – including enhanced team-wide accountability, regular manager-employee oversight and mentorship, decreased staff absenteeism. Implementing the PPP has also come with challenges, which provide important learning for the future of the healthcare sector.
Our initial experience with PPP management at Charikot has demonstrated improved effectiveness of the public-sector healthcare system, with increased service delivery, higher quality of services provided, expanded learning opportunities, and enhanced management structures. Yet it has also experienced challenges, including effective stakeholder collaboration, lack of clarity surrounding PPP policy, and effective mechanisms to integrate staff.
Overall, however, patients in the Dolakha district have benefited greatly from the PPP at Charikot, and while challenges remain, we are optimistic about the PPP model’s ability to provide high-quality public-sector healthcare.
As in other sectors throughout Nepal, the PPP model offers tremendous potential value to the healthcare system. Importantly, the PPP model also offers us the opportunity to guarantee the Constitutional right to healthcare for all citizens.
As we look forward to a healthcare system that can provide citizens throughout the country affordable, high-quality healthcare, the lessons from the Charikot experience must be heeded.
Working together across sectors, we can build a better and more equitable Nepal, where quality healthcare is guaranteed.
Kalaunee is the Director of Governance and Partnerships for Possible (Nyaya Health Nepal), Regmi is Chief Specialist, Ministry of Health and Schwarz is faculty at Harvard Medical School (Boston, USA)