Dengue outbreak
Presently, hundreds of patients with dengue infections are being admitted, and dozens of others are being treated at the outpatient department of Sukraraj Tropical and Infectious Disease Hospital (STIDH). Outbreak of dengue was first noticed in September in Sarlahi district this year. So far, patients from more than 14 districts, including Kathmandu, Bhaktapur and Lalitpur, have been treated at STIDH. It seems that dengue is spreading at an alarming rate from the Southern to Northern parts of Nepal.
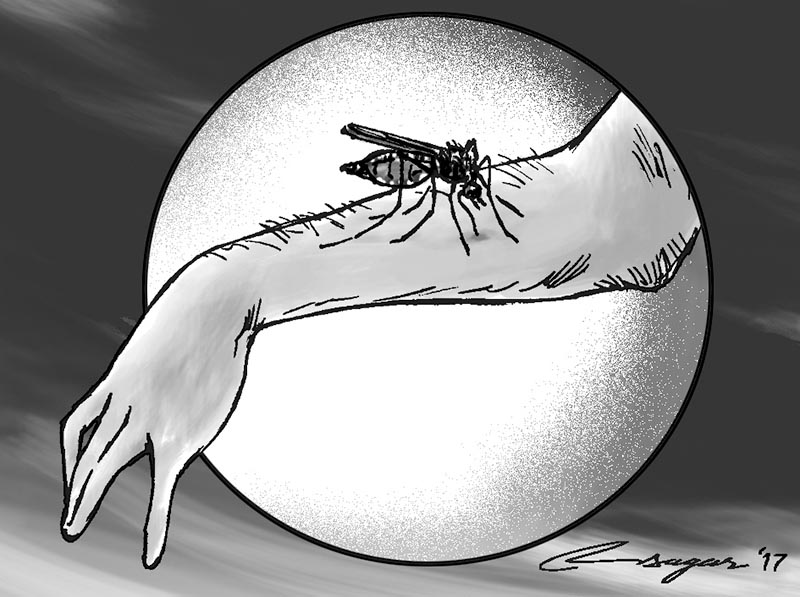
Dengue is an emerging, but a relatively new known disease in Nepal. It was first described in 2004 in Nepal. Since then, major dengue outbreaks have been occurring at two to four-year intervals in Nepal. Each year, outbreaks are expected to occur from September through November. During this period, dengue virus carrier mosquitoes known as Aedes agypti and albopictus are more active, especially during daytime.
These mosquitoes were previously thought to be restricted to southern Tarai region; however, nowadays it is becoming more and more apparent in hilly regions of Nepal. Although dengue outbreak is expected during the post-monsoon season, policy-makers, government-concerned body, and even the general public usually do not take or follow its preventive measures sincerely.
As a result, during dengue epidemic, every year a large number of patients with dengue viruses are admitted or visit hospitals across the country. During that time, there has always been a sharp shortage of detection kits, while rapid response teams are usually dispatched to dengue-affected areas only after outbreaks have occurred.
Unfortunately, by that time, hospitals have to struggle to cope with an overflow of hundreds of dengue patients in affected areas. Currently, everyday STIDH is receiving dozens of patients with dengue like illnesses from across the country and almost all are found positive for dengue virus by laboratory testing.
Laboratory testing is necessary to confirm dengue virus in patients with fever because other bacterial or viral infections can cause similar symptoms to those of dengue. At present, rapid diagnostic test (RDT) kits are widely used by hospitals for the confirmation of dengue virus in Nepal.
Nonetheless, inaccurate identification of the virus is one of the main drawbacks of RDT kits. In a recent research, it is has been demonstrated that nearly half of the dengue virus positive cases using RDT kits, are later turned out to be Zika virus. At least tertiary hospitals should, therefore, perform PCR method (latest technology) to definitely confirm the virus. It can also distinguish its serotypes, which is helpful in predicting outcome of the disease. As a matter of fact, subsequent infections with a different serotype increase risk of the severe disease. So far, government of Nepal do not perform regular serotyping in a routine test. Fever, pain behind the eyes, severe joint pain, muscular pain, nausea, vomiting, and rash are the main symptoms of dengue fever. Severe abdominal pain, persisting vomiting, bleeding from nose or gums, lethargy and restlessness are warning signs of dengue fever. Approximately 10% of the cases develop warning signs.
A patient with warning signs requires hospitalization. Severe bleeding, shock, fluid buildup in the abdomen or chest with respiratory distress, other organs such as liver, central nervous system, heart involvement are considered as severe dengue infection. Patient with severe dengue need urgent treatment. Symptoms usually begin, four to 10 days after the infection. Early identification of dengue symptoms not only helps prevent its complications but also prevents it from spreading to other parts of the country.
No specific treatment is available for dengue virus, but possible complications are cause for concern. In many cases, physical condition looks stable, but they may have abnormality in laboratory results, meaning patients may develop critical condition without having warning signs or symptoms.
Thus, physicians depend heavily on accurate blood results in predicting disease progression and outcome of dengue patients. A white blood cell, platelet count, hematocrit count and liver function tests are essential to understand the condition of a dengue patient. Rapid decrease in platelet count and rising in hematocrit indicate a possible serious health consequence in a patient with dengue infection.
According to the Indian dengue guideline, platelet blood transfusion are not required in stable patients with platelet count below 20,000/cumm but they require transfusion if below 10,000/cumm. Nevertheless, we do not have our own criteria for blood transfusion that is based on our local research.
In the past, platelet blood transfusion was usually found in short supply during dengue epidemics. Past experience shows that large dengue epidemics is almost inevitable at two to four-year intervals in Nepal, particularly in Southern Tarai region of Nepal, which results in high demand for platelet blood in the coming years.
Dengue epidemic is currently present throughout the country, and it is experiencing its largest outbreak since 2010. This epidemic could have been prevented had the government implemented preventive measures immediately following the end of the rainy season.
Pun is Coordinator of the Clinical Research Unit, Sukraraj Tropical and
Infectious Disease Hospital