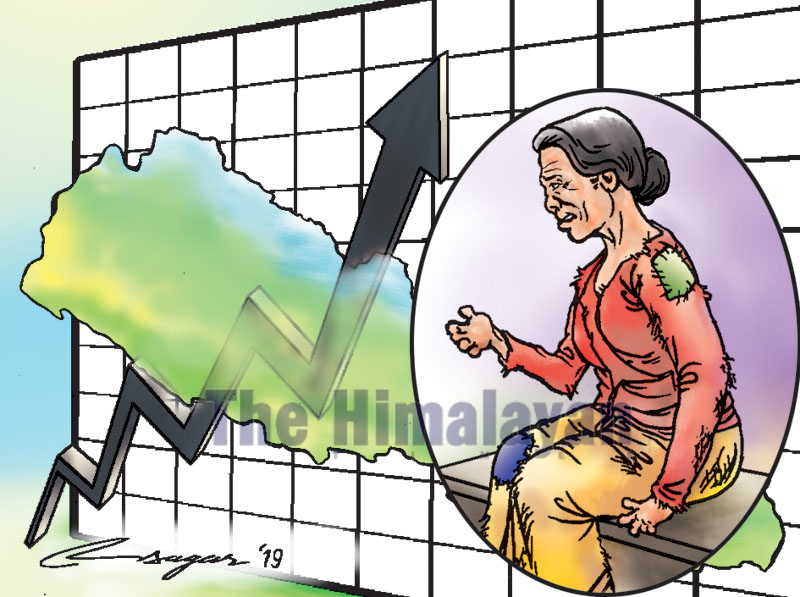
Increasing leprosy cases
The country’s transition to federalism has jolted the leprosy services at the local, provincial and national level. Leprosy is not a priority at the local level, and the budget is not adequate for potent interventions
Every two hours and forty minutes, a new leprosy case was detected in 2018 in Nepal. Out of 77 districts in the country, 21 districts are categorised as high leprosy endemic districts, with a leprosy prevalence rate (PR in 10,000 population) higher than 1.
All districts except Saptari in Province 2 had a leprosy PR of more than 1, with 1,177 new leprosy cases confirmed in 2018 alone. Province 5 and Sudurpashchim Province also had a leprosy PR greater than 1. The leprosy burden in children was quite conspicuous, with 202 cases diagnosed in 2018.
Deformity due to leprosy is the vital burden, as Grade 2 disability (visible impairments and deformity) was detected in 87 cases in 2017 and 133 in 2018. This means early leprosy detection and treatment strategies are inadequate in Nepal.
Globally, the elimination of leprosy as a public health problem was achieved in 2000. However, new leprosy cases diagnosed globally is still significant. Nepal lies in the high leprosy burden in the South-east Asia region and was ranked as one of the 23 highest leprosy burden countries in the world in 2018.
Leprosy elimination was achieved in 2010 in Nepal; however, the national leprosy PR and district-wise leprosy burden have been rising in the last five years. Leprosy endemic districts increased from 17 to 21 from 2017 to 2018 due to active case detection activities.
Leprosy, also known as Hansen’s disease, is an infectious disease, caused by a slow-growing type of bacteria, Mycobacterium leprae. Leprosy predominantly affects the skin and peripheral nerves, resulting in neuropathy and associated long-term consequences - deformities and disability. Stigma is attached to the disease even today when deformities are present. Leprosy previously was considered as an incurable, mutilating and contagious disease.
Published research studies reveal that approximately 95% of patients exposed to M. leprae never develop the disease due to the natural immunity. Leprosy is one of the potent 20 neglected tropical diseases, known to occur at all ages mostly in low, middle-income countries. Multidrug treatment (MDT: Rifampicin, Dapsone, Clofazimine) is very effective in the treatment of leprosy.
The country’s transition to federalism has jolted the leprosy services or activities at the local, provincial and national level. Leprosy is not a priority at the local level, and the health staff are burdened with additional health activities. The leprosy budget is not adequate to address the overall demands of potent programmes and interventions. Although Nepal has adopted a national leprosy strategy, from a global leprosy strategy, 2016-2020 for leprosy prevention interventions, effective implementation has been limited, particularly in high endemic districts.
Social stigma is a key factor for the delay in diagnosis and treatment and incomplete follow-up.
To resolve the existing challenges and burdens in leprosy, the government, in collaboration with NGOs and INGOs working directly or indirectly on leprosy, has been engaged in early leprosy detection and treatment. As a result, 190,000 patients have undergone MDT since 1982.
However, around 30,000 people still live with disabilities due to delayed diagnosis of leprosy.
For leprosy prevention in Nepal, the government is recommended to go for an effective early case detection system and treatment. This requires intensifying active case finding for reducing disabilities; categorising leprosy endemic districts and local levels; strengthening leprosy awareness and stigma reduction; and an effective treatment system.
The government must also enhance leprosy prevention and management by maximising contact (with priority on children (screening and providing the chemoprophylaxis drug; strengthening the supply chain management for uninterrupted supply of leprosy care medication and appliances; and expanding access to comprehensive disability care in public facilities.
Effective training, capacity building and resource personnel must be strengthened through training of health professionals, strengthening technically qualified resource staff and health professionals at the district, municipality and community levels. Increasing funding and research for leprosy prevention are a must. This can be done through partnerships for mutual funding and strengthening research activities for better leprosy diagnosis, prevention and treatment.
There is a need to strengthen partnerships through active mutual engagement in effective planning and implementation of leprosy prevention interventions. The government is recommended to strengthen effective surveillance for leprosy recording and reporting (digital system) and enhance analysis and feedback.
There is also a need for advocacy to continue high priority leprosy programmes and abolish the existing leprosy discriminatory law.
Nepal may not achieve the National 2020 target of eliminating leprosy at the district level. Only reinforcing the national leprosy programme to engage provinces, municipalities and multi-sectoral partners for enhancing early case detection, effective treatment and management with full-fledged political commitment will help attain zero new leprosy, zero disability and zero discrimination.
Dr Dulal is a research scientist