Health for all: Meeting the challenge
Under federalism, there is a greater need for health system reform to ensure better alignment with the broader national policies, targets and SDGs. The power of digital health technologies must also be harnessed to ensure health services for all
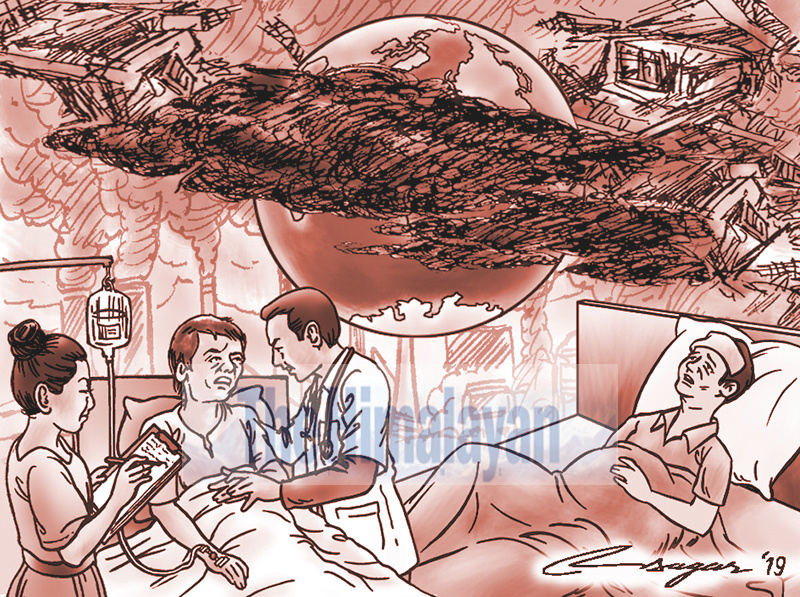
The global health environment is becoming complex in the recent years. Social, demographic and epidemiological transformations have profound impacts on human health. The right of every individual to basic health services is an important priority. Therefore, health for all is a crucial agenda for achieving the Sustainable Development Goals (SDGs).
To this end, strategies are being implemented to advance universal health coverage in most of the developing countries. Universal health coverage implies that all people have access to quality health services without any financial hardship. This approach focusses on primary health care, which is a cost-effective and equitable way of delivering health services. Therefore, ensuring universal health coverage is key to meeting the social goal of health for all.
In order to have a better sense of who is missing out, we need reliable and credible data on several social, economic, cultural, physical and political factors that significantly affect access to health services. Therefore, a critical analysis of the social determinants of health can be useful to address the key barriers in accessing essential health services.
Like many developing countries, Nepal has formulated a number of health policies, strategies and plans to improve the health status of the entire population. A systematic review of the national health policies shows that most of them are found to focus on governance and service delivery. However, more emphasis on equity and multi-sector approach would be effective in improving health sector performance at all levels.
Though strengthening the health system is a key priority for the policy makers, the progress is still slow so far. Therefore, it is high time to effectively engage with national budgetary authorities to enhance credible, priority-oriented health budgets, and ensure efficient fund flows to the local levels.
At this stage, more concerted efforts are needed to advance a robust financing mechanism that will ensure well-trained human resources for health and enhance evidence-informed decisions for policy making. Apart from this, national health strategies should focus on cost-effective interventions for most marginalised and disadvantaged populations. Considering the geographical diversity, more investments are needed to improve access to and utilisation of quality maternal, newborn and child health services in remote areas.
Additionally, more targeted interventions are needed to provide health care services for people living with HIV, TB and malaria. Despite some progress, there are some resource gaps to meet the unmet needs of health services to the vulnerable populations. Furthermore, more reliance on external funding creates dependency on donors, which will have creeping impacts on local ownership and sustainability of health services.
As Nepal has now transitioned to a federal structure, there is a greater need for health system reform to ensure better alignment with the broader national policies, targets and SDGs. More importantly, it is high time to harness the power of digital health technologies to ensure health services for all.
In the changed political context, the role of the development partners is instrumental in strengthening the capacity of the government to implement a range of health policies which aim to respond to the health needs and priorities at all levels. Better coordination and collaboration among the development partners, private sector and civil society organizations are crucial to support the government’s efforts in achieving the targets and objectives of the health policies.
On the other hand, there is a need for equitable distribution of the health workforce across the country. For this, there are emerging priorities of effective implementation of health policies and strategic plans in a participatory and gender-sensitive approach. Because our ultimate goal is to ensure robust, efficient, evidence-informed health systems that provide quality health services to all people.
At the national level, recent policy dialogues and multi-stakeholder consultations have been helpful in designing strategic roadmaps for interventions to address the existing gaps and challenges in the health sector. However, the Ministry of Health and Population must pay more attention in ensuring effective implementation of these strategic interventions to improve health sector performance.
Undoubtedly, all people will be affected by climate change and environmental degradation. But children and elderly people are the most vulnerable. Similarly, natural disasters, varying rainfall patterns and changing weather conditions are affecting the health and livelihoods of poor and vulnerable populations. Increasing trends of non-communicable diseases is another worrying challenge in terms of investments.
That being said, public health is a vital issue for sustainable development. Political commitment is crucial to enhance social accountability in the health sector and improve the health and well-being of all people. Indeed, the poor performance of health systems is increasingly becoming a political concern that requires integrated and people-centred health services.
Bhandari is PhD candidate in Public Health at Chulalongkorn University, Thailand