Efficacy of rapid corona tests questioned as 16 test positive after negative RDT
Kathmandu, April 24
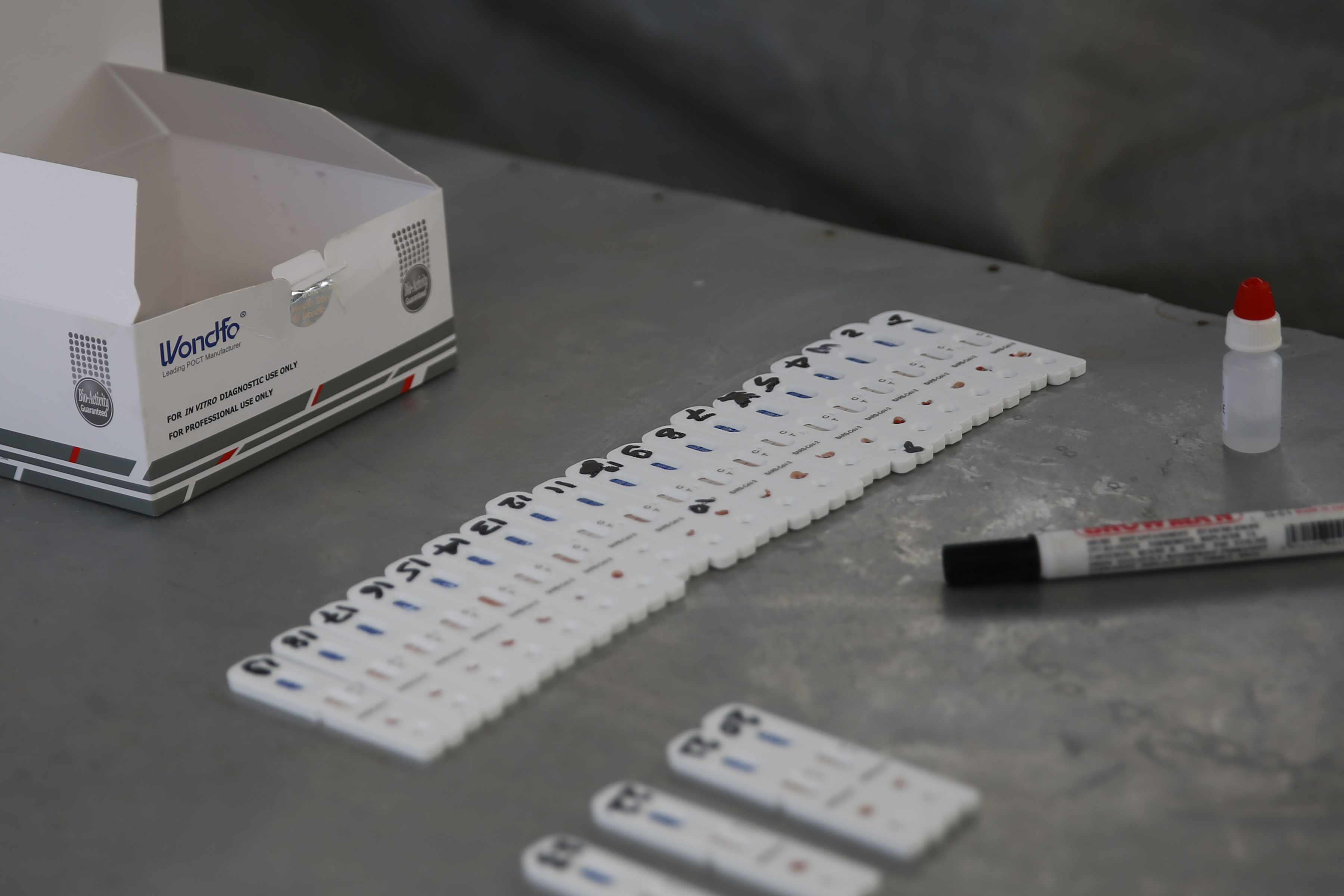
The efficacy of the rapid diagnostic tests in confirming coronavirus infection has been called into question, as all of the 16 coronavirus tests performed on patients living in Nuri mosque in Udayapur district had generated faulty results. Fortunately, they were later asked to undergo polymerase chain reaction tests as well, which finally confirmed the infection.
Nuri mosque is now considered the epicentre of coronavirus infection in Udayapur district, as many of the people who came into contact with those residing at the religious site have contracted the disease. Udayapur now has 28 coronavirus positive patients. They are undergoing treatment at Coronavirus Special Hospital in Biratnagar.
“Health experts have warned that making clinical decisions with RDT can be counter-productive,” said a doctor on condition of anonymity. “They say RDT should only be used to find out prevalence of COVID in the community. To identify and isolate coronavirus patients, PCR tests must be performed as they can detect the disease at a very early stage of infection.”
Questions about accuracy of rapid diagnostic tests have been raised worldwide. On Tuesday, India’s health research agency suspended the use of rapid antibody test kits procured from China for two days after the accuracy of these tests swung wildly from six per cent to 71 per cent.
Rapid diagnostics tests are not reliable as they deliver results based on presence of antibodies in the blood of COVID suspects.
“A human body generally generates antibodies after seven to 14 days of getting infected. If rapid tests are conducted within this period, even people infected with COVID-19 will be declared infection-free because of lack of presence of antibodies,” said Shravan Kumar Mishra, virologist at National Public Health Laboratory. “That’s why PCR test is much more reliable as it detects specific genetic material within the virus, which can be seen immediately after it enters the human body.”
According to the World Health Organisation, majority of patients develop antibody response only in the second week of onset of symptoms. The WHO does not recommend the use of antibody-detecting rapid diagnostic tests for patient care, but encourages continuation of work to establish their usefulness in disease surveillance and epidemiological research.
The government has so far conducted 47,496 tests to confirm coronavirus infection. Of these tests, 80 per cent, or 38,089, were rapid diagnostic tests.
“Only 10 per cent of the people who have undergone RDT are asked to perform PCR tests,” said Samir Kumar Adhikari, chief of Health Emergency Operation Centre at the Ministry of Health and Population. “But we are planning to extend PCR tests in the coming days.”
A protocol of the health ministry states, “If the test was done by RDT, repeat the test using PCR only for positive cases. If test is negative but symptoms persist, then PCR is recommended.”
This means a person who has undergone rapid test will be asked to perform PCR test only if he or she shows symptoms of COVID-19. However, over 80 per cent of the coronavirus patients in Nepal are asymptomatic. This probably means that many asymptomatic coronavirus infected patients, who underwent RDT and tested negative, may be moving freely in society. “
A person who tests negative in RDT but tests positive in PCR is a risk as there are chances that the person could infect others. So, RDT results should not be accepted as final,” said epidemiologist and public health expert Sujan Marahatta.
A version of this article appears in e-paper on April 25, 2020, of The Himalayan Times.