Patients with fever being turned away due to COVID fear
Kathmandu, April 1
A 52-year-old woman lost her life in Biratnagar yesterday after a number of hospitals declined to admit her on suspicion that she had contracted coronavirus infection.
The woman suffering from high blood pressure had a fever of 102 degree Fahrenheit when she was rushed to BP Koirala Health Science Academy in Dharan. The academy said she had to be admitted to the intensive care unit and referred her to Neuro Hospital in Biratnagar, stating it did not have a vacant ICU bed. The Neuro Hospital then referred her to Birat Nursing Home, which, in turn, referred her to Nobel Hospital. She breathed her last within one-and-a-half hours after getting admitted to Nobel Hospital as she failed to receive medical care on time.
This is not the first time a life has been lost because of mere suspicion that the patient might be suffering from coronavirus infection.
A 20-year-old man from Dhoda of Kalaiya sub-metropolitan city died on Monday after Birgunj-based hospitals refused to treat him, saying that he was suffering from coronavirus disease. The man, who had received injuries and cuts while he was threshing red lentils, was taken to Birgunj National Medical College Teaching Hospital on Saturday after he complained of fever.
The hospital hold him the next day that he was infected with COVID-19 and used police force to throw him out. He visited other hospitals in Birgunj, but they declined to treat him as BNMCTH had told them about his health condition. So he was rushed to Tribhuvan University Teaching Hospital in Kathmandu, but it was too late. A COVID-19 test performed by TUTH on the man later turned out to be negative.
The primary duty of medical professionals is to provide care to all the patients who come to them without any discrimination and to do the best to save people’s lives. This is their social as well as professional duty. But ever since the number of people infected with COVID-19 gradually started to go up in Nepal, many doctors across the country, including in Kathmandu valley, have started refusing to attend to patients with fever and dry cough.
A few days ago, a UAE-returnee suffering from fever and breathing difficulty was admitted to the newly-established corona isolation hospital in Butwal on suspicion that he had contracted the deadly infection. He later tested negative for COVID-19. But by that time, he had passed away as the corona isolation hospital did not have an ICU and ventilator.
Now doctors say he probably would have survived had he been admitted to a well-equipped hospital.
As hospitals are refusing to admit patients with symptoms akin to COVID-19, pressure is mounting on Sukraraj Tropical and Infectious Disease Hospital, which has been designated by the government for treatment of coronavirus disease.
“We have been receiving five referral cases of patients with fever every day from other hospitals,” said STIDH Spokesperson Anup Bastola.
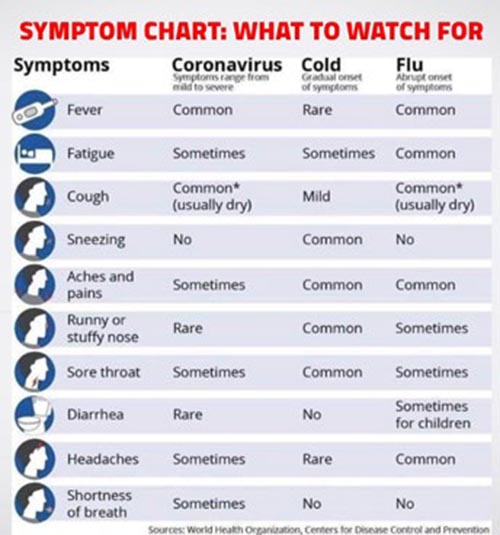
“Doctors should understand that there is always a difference between COVID-19 patients and other patients with fever. Coronavirus patients generally have dry cough and have difficulty breathing usually in the evening which gradually progresses.”
A patient, who is suspected of contracting COVID-19, according to Bastola, should have a travel history and should have come into contact with those who have come from foreign countries where there is community transmission.
“Therefore every person with fever should not be treated as a COVID-19 patient,” said Bastola.
Fever may be associated with many other diseases such as dengue and malaria, said Basudev Pandey, director at Epidemiology and Disease Control Division under the Department of Health Services.
And this is the time of the year when people suffer from dengue and malaria. “So, doctors should not randomly refer all patients with fever to STIDH,” Pandey said.
These instances show that doctors may be lacking ‘knowledge about coronavirus infection’, said Anup Subidee, consultant infectious disease physician and public health expert at HAMS hospital.
“But what is also true is that health workers are facing shortage of personal protective equipment, exposing doctors and nurses to risk of contracting COVID-19,” added Subidee. “However, it is ethical duty of doctors to treat the patients as well.”
Nepal Medical Council, a statutory body that provides licence to practice medicine, has also said the government should provide PPE to health workers. “If a complaint is filed with evidence that a hospital had referred patients to another hospital without offering medical treatment, we will take action,” said Bishwa Dawadi, NMC chief of the Ethical Committee.